All essential workers, particularly health care professionals and first responders, deserve our gratitude for doing what needs to be done in this scary time of physical distancing and the unprecedented COVID-19 pandemic.
As the number of COVID-19 diagnoses rises every day in the US, what the public may not realize is that full recovery from coronavirus disease, or COVID-19, usually doesn’t happen in a hospital. It happens in your community. In your own backyard.
Most confirmed cases of COVID-19 are never hospitalized. And those who are, when their symptoms stabilize, discharge home to finish their full recovery. Still “active,” still in isolation.
Enter Hope Cochran, RN, a BAYADA Home Health Care Nurse in Wilmington, Delaware. She provides short-term home nursing visits to help clients recover from a hospitalization—usually a surgery or acute event—or to help them better manage a chronic condition such as diabetes or COPD. Now, in this viral outbreak and public health emergency, she also helps clients recover from COVID-19.

She took time out of a busy day to share her frontline view of how COVID-19 is affecting their community.
Could you describe for us, first, the community or neighborhoods you serve?
We serve Wilmington, Delaware, and its surrounding counties. At least half of my personal territory live in high-rise apartment buildings here in the city.
And what kinds of COVID-19 care have they needed?
I’ve had three so far, and it depends on the severity of their symptoms. One required oxygen support; two do not. One was a client with dementia who couldn’t don a mask or understand why they couldn’t be near other people, and they had to move in with family because the assisted living facility couldn’t allow them back with coronavirus.
I’d say most of it involves respiratory education—teaching them the warning signs to look out for, like shortness of breath, cough. Taking temperatures. Reinforcing the education they got in the hospital about their symptoms. Teaching them over again how to self-isolate and prevent infection, because that can be tricky sometimes, and they’re not always fully compliant if we don’t keep an eye out. And a lot of it is emotional support, just asking them open-ended questions to see how they’re doing and helping them cope.
For the clients who were previously independent, now their needs relate to a lack of endurance. You spend one day in the hospital, you lose three days of muscle mass. They’re weak and deconditioned, so I help them with their ADLs (activities of daily living) and rebuilding their strength.
Were you scared at first, caring for this population?
Well, I’m not going to lie, this was a decision I didn’t take lightly. I thought about it very seriously. But I thought, if this is what’s coming, I want to be as educated as possible. Since I have the opportunity, if I can do this now, then it’s the best choice for our team. I can use what I’ve gained to make it easier for the rest of our nursing teams. That’s the goal.
It’s been intense; there’s a lot to think about. But now, I feel my regular clients are probably safer from coronavirus than most other people because I take so many precautions. And I usually see COVID-positive clients only two times a week to every other week, depending on severity. Always at the end of my day, so I can go home and do what I need to do to stay safe.
Do you feel like you have everything you need to protect yourself and others?
Our office is so supportive of our clinicians, they really go out of their way to make sure we’re up to date on changing clinical guidelines. They come out and deliver supplies straight to my car, like a drive-through. PPE (personal protective equipment), bags, pens—because you have to leave your pens there—I never once felt like I didn’t have what I needed to care for these and other clients.
The invisible part is everything our team does before the client even comes home! While they’re still in the hospital, our community liaison is making sure they have responsible family caregivers at home who are well educated. They’re working with the CSM (client services manager) and CM (clinical manager) to ask, “Do you have these symptoms? Do you have internet? A trash can, a table we can use? Do you have six feet of space?” And they find all the resources they need. It’s a lot of preparation and education upfront to make sure my visits run smoothly.
What do you think would happen to them—where would your COVID-positive clients be if they couldn’t get home health care services?
Oh no doubt, they’d be right back in the hospital. And maybe not even for COVID-19, but it’s all the comorbidities that make this challenging.
What are some things about home COVID-19 care that you think would surprise our readers?
I think one of the biggest misconceptions is that you’re discharged from the hospital, you must be good. But they’re not. No matter what your diagnosis is, people are released from the hospital sick. The scope of it with COVID-19 is much more than people realize, especially in the home.
Our COVID-positive clients have needed so much more care than I ever expected. The clients and their families need so much teaching and follow-up. Most of my clients are elderly, their caregivers are elderly, and in the city they don’t have the resources to Zoom, or to download apps. They can’t use telehealth with their doctors without assistance. Home nurses are their conduit to everything else that keeps them healthy and safe.
It is so important we have the PPE and supplies and clinical support we need to provide this care. Because think about it; you’re COVID-positive and in isolation. If your family member doesn’t take the right precautions, then that isolation period becomes extended; you have to add 14 days now for that caregiver’s exposure. If they don’t understand that, they could be taking the virus out into the community. This is so important. Look outside, look at who is home right now. They are your elderly parent, your neighbor, and everyone’s in close proximity. We have to provide home care to keep everyone safe, out of the hospital and not using additional resources.
So what would you say to other nurses providing COVID-19 care for the first time?
I’d tell them overall, my experience has been positive. You have to use your support team, the PT (physical therapist) and OT (occupational therapist) who are also providing care, everyone in your service office—we’re constantly bouncing ideas off each other, and it’s definitely a full team effort, across the board.
While this may be a new foe, we know how to do this. No one has ever done this before, but nurses are a wealth of knowledge. We’re trained for this—we can maintain our safety and the safety of our clients and families.
Talk to your teammates about what worked well, what didn’t, so you don’t feel overwhelmed. We provide home care independently, and that’s part of what I love about this job, but we’re not working in a vacuum. We have each other’s support—we have friends who care looking out for us, who want to make sure we have everything we need to keep ourselves and everyone else safe and protected.
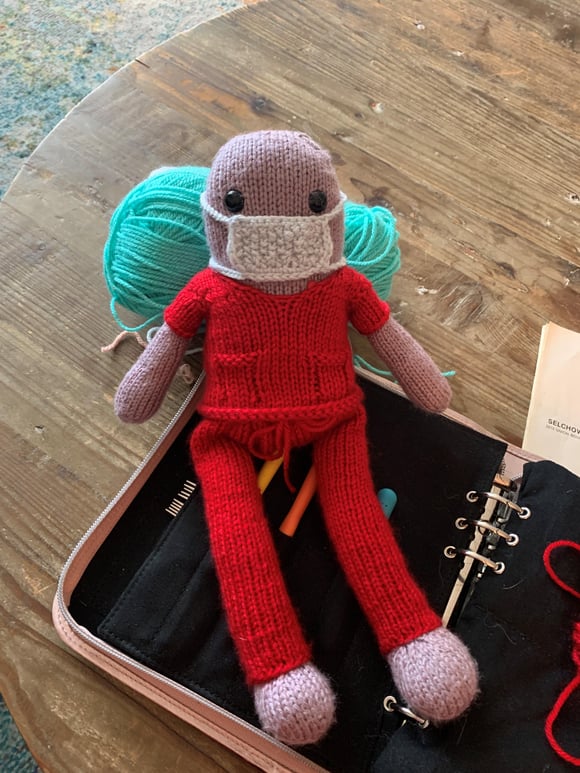 To relax at night, Hope just finished knitting a face mask and scrubs for her Kirby Wirby doll.
To relax at night, Hope just finished knitting a face mask and scrubs for her Kirby Wirby doll.


Let Us Know What You Thought about this Post.
Put your Comment Below.