Often referred to as a noble profession, nursing can be as demanding as it is rewarding. The continued responsibilities and stressors that go along with the work can lead to burnout, which often affects the quality of care, patient safety, job satisfaction, and emotional wellness. Burnout is a fairly common occurrence among nurses, with approximately 38% of nurses reporting experiencing burnout at some point in their career.
So how you can avoid burnout? First, it’s important that you recognize the early signs and symptoms of burnout and implement changes that can help you regain your sense of self and control. It’s also critically important that your supervisors and other health care leadership readily identify the signs so they can offer the needed support, helping to stop burnout in its tracks.
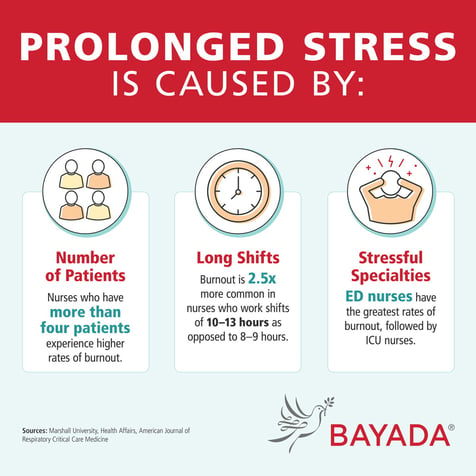
Prolonged stress is caused by:
Number of patients: Nurses who have more than four patients experience higher rates of burnout
Long shifts: Burnout is 2.5 times more common in nurses who work shifts of 10-13 hours as opposed to 8-9 hours.
Stressful specialties: ED nurses have the greatest rates of burnout followed by ICU nurses.
sources: Marshall University Health Affairs, American Journal of Respiratory Critical Care Medicine
Causes and warning signs of nursing burnout
The signs and symptoms of nursing burnout can vary widely depending on the individual—they can manifest themselves physically, emotionally, and behaviorally:
- Physical burnout: Excessive job demands, staffing shortages resulting in longer or too many shifts, increased responsibilities, as well as insufficient job resources can all lead to physical exhaustion. Symptoms include:
- Anxiety
- Insomnia Frequent illnesses
- Headaches
- Muscle pain
- Changes in appetite
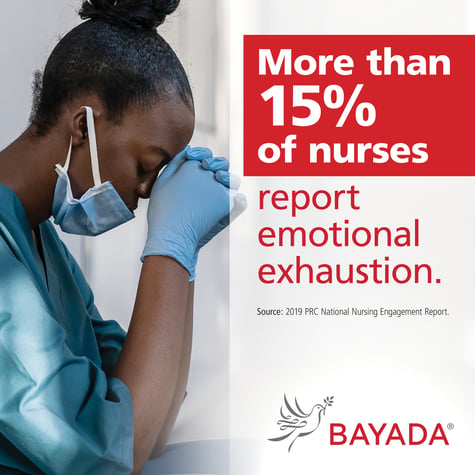
- Emotional burnout: Excessive and prolonged stress can impact the level of care a nurse provides not only to their patient, as it can several impact their emotional well-being. Symptoms include:
- Feelings of helplessness and depression
- Self-doubt or sense of failure
- Decrease in job satisfaction or motivation
- Dreading work
- Lack of empathy or insensitivity
- Behavioral burnout: Nurse burnout or compassion fatigue can ultimately affect a nurse's behavior which becomes noticeable not only to the client or patient but other staff members. These changes can be exhibited in many forms, including but not limited to:
- Attitude and behavioral changes (apathetic, irritable, cynical)
- Impaired ability to make well-informed decisions
- Increase in work absences or showing up late
- Decreased productivity
- Substance abuse
Is compassion fatigue the same thing as burnout?
Nurse compassion fatigue is deeply physical and spiritual exhaustion—accompanied by emotional pain—from providing care for patients. It is extremely widespread among health care professionals, particularly if they work intimately with elderly patients and those suffering from terminal illnesses. The signs and symptoms are similar to burnout, but at a much more extreme level.
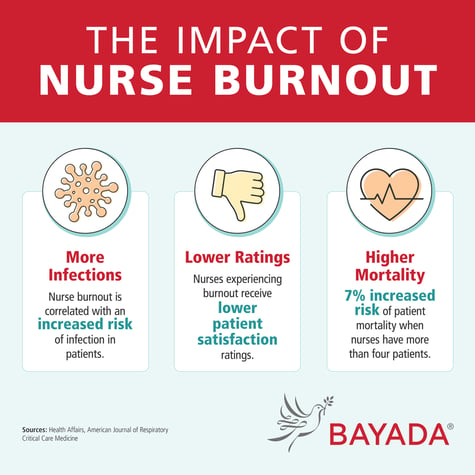
More Infections: Nurse burnout is correlated with an increased risk of infection in patients
Lower Ratings: Nurses experiencing burnout receive lower patient satisfaction ratings.
Higher Mortality: 7% increased risk of patient mortality when nurses have more than four patients.
sources: Health Affairs, American Journal of Respiratory Critical Care Medicine
Tips for preventing burnout
Though you may feel overwhelmed by your situation, know that there are things you can do to prevent or reduce the effects of burnout. Here are some tips:
- Seek out help. When and if you start to recognize a change in your behavior (a co-worker may also tell you), take advantage of the support systems that are in place whether through your organization or a personal mental healthcare provider.
- Take control of your schedule. Consider taking time off, reduce your hours temporarily, or ask to work in a different setting or with other patients.
- Get enough sleep. Sleep deprivation exacerbates and contributes to physical distress.
- Sticking to a regular exercise routine—even if it's just taking in a good walk during your work breaks, as well as eating a well-balanced diet can help to reduce physical exhaustion.
- Practice self-care and mindfulness. Do whatever helps you relax and recharge: get a massage, meditate, do yoga.
- Do things outside of work that make you happy. Engage in the things you love to do and be with people who make you feel most happy, fulfilled, and supported.
Self-care is needed for mental health wellness
Just as an airplane crew instructs you to put your oxygen mask on first before helping others, you need to make sure you are taking care of yourself before you can be successful in helping others. Though common for health care professionals to put their patients first and themselves last, it is critical to prioritize your own mental health and work boundaries to reduce the chances of experiencing nurse burnout. In other words, prioritize your own well-being!
Bureau of Labor Statistics, “Registered Nurses,” Occupational Outlook Handbook, last modified April 2020: https://www.bls.gov/OOH/healthcare/registered-nurses.htm
Kronos, “Wake Up to the Facts About Fatigue,” 2018: https://www.kronos.com/resource/download/24266
Ekaterina Gutsan et al., “Burnout syndrome and nurse-to-patient ratio in the workplace.” April 2018: https://mds.marshall.edu/cgi/viewcontent.cgi?article=1196&context=mgmt_faculty
“Nurse Burnout: Risks, Causes, and Precautions.” University of St. Augustine for Health Sciences, September 9, 2021. https://www.usa.edu/blog/nurse-burnout/.


Let Us Know What You Thought about this Post.
Put your Comment Below.