When most of the population is asked to isolate in their homes and practice social distancing, there are some who have to face this crisis head-on: doctors, nurses, home health aides, and other caregivers—you. You’re there to answer the call every day. For that, we thank you.
To honor you and your hard work all across the health care industry, we gathered some tips and reminders to help you stay safe and curb the spread of the Coronavirus (COVID-19).
1. Use the right mask for the right task.
Providers industrywide are still scrambling for them and other PPE supplies, so explaining the differences may seem tone-deaf to people who’ve been trying to get their hands on them. We know that, and we sympathize, but we still have to clear up some misconceptions—the first being that everyone needs to get their hands on one immediately.
 The truth is: we’ve all got to be deliberate about conserving masks and other PPE for the situations where they’re medically required for employees caring for COVID-19 positive/exposed clients. Hopefully this section helps clarify what masks you should use for the situations you’re in.
The truth is: we’ve all got to be deliberate about conserving masks and other PPE for the situations where they’re medically required for employees caring for COVID-19 positive/exposed clients. Hopefully this section helps clarify what masks you should use for the situations you’re in.
So, there are three types of masks we’re going to discuss here: PPE-grade ones, like N95 masks and surgical masks, and then non-PPE masks, or “comfort” masks, as we call them at BAYADA.
Non-PPE/Comfort Masks
These are the masks you can buy at any Target or Walmart (provided that they’ve been restocked after they initially flew off the shelves). You may have even seen these on social media being sewn by people who are concerned and want to give back during this health crisis. But both store-bought (unless it clearly says PPE-grade) and homemade masks do not effectively protect the wearer from the virus.
So what can comfort masks be used for?
Well, as the name implies—the presence of a mask can decrease your anxiety and the anxiety of your patients, too (especially if they demand you wear a mask, even when it’s not medically-required).
It’s also not a bad idea to use them as a reminder: don’t touch your face, try to wash your hands more than seems necessary, and be extra vigilant in your infection prevention practices. Just make sure you’re disinfecting your hands before handling the mask and after you remove it—and change your mask as soon as it gets moist.
For more information on how to safely use comfort masks, click here.
Surgical Masks
Use these PPE-grade surgical masks (and double check that they are) when you’re taking droplet precautions with a patient. Droplet precautions are used with patients sick with influenza, respiratory syncytial virus (RSV), adenovirus, pertussis, mumps, rubella, and other upper respiratory infections where secretions aren’t contained.
At BAYADA, we’re asking people to use their surgical masks (and other necessary PPE—refer to our PPE guidance one-pager here) when caring for asymptomatic clients with known exposure and asymptomatic or symptomatic clients awaiting test results.
N95 Masks
N95 Masks should only be reserved for positive COVID-19 clients. You don’t want to waste a mask on a client who just has seasonal allergies, when they are absolutely essential to protect against COVID-19 transmission.
However, you shouldn’t be wearing a N95 mask if you haven’t been fit-tested, and you can’t be fit-tested (at least, at BAYADA) without receiving medical clearance first. Reach out to your supervisor for medical clearance, so you can get the ball rolling.
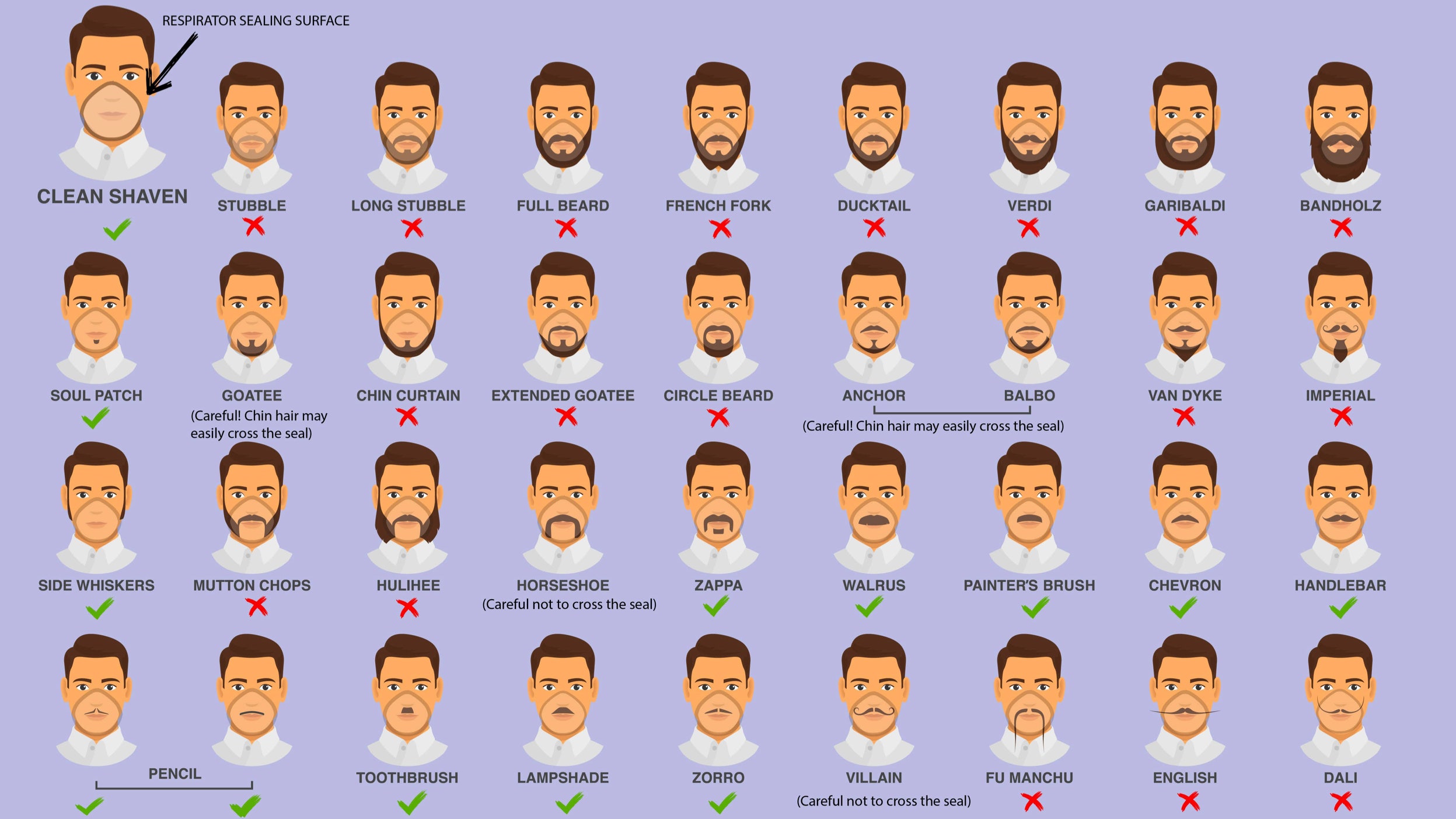
What is fit testing and why is it so important? Fit testing ensures that the N95 mask is customized to your face so a seal forms, protecting you against transmission. For those of you with facial hair, you may need to shave. See the CDC graphic below.
If you’re wearing an N95, you’re also probably equipped with a gown, goggles, and other items of PPE. Click here for a refresher on the appropriate way to don your PPE and to remove it.
2. Think about your glasses as the “comfort” mask of eyewear.
Goggles are a necessary addition to your PPE wardrobe, especially if you’re treating a patient positive for COVID-19. But wearing your regular glasses can be a method of practicing airborne precautions all the time—at home and at work. You’re adding an extra layer of prevention from any airborne COVID-19 droplets, provided that those droplets are traveling at you head-on. Even if they’re not all that effective in a clinical sense, they can act as another reminder to not touch your face.
But always use infection prevention techniques: clean your glasses regularly, disinfect before putting them on, and again after removing them.
3. Don’t touch your face!
This was all anyone could talk about mid-March, when the President remarked that he “[hadn’t] touched [his] face in weeks.” Though the talk has died, the practice shouldn’t.
We all touch our faces more than we’d like to admit—or even realize. It’s a habit—and, as with any habit, it can be broken. First, you’ve got to figure out what triggers the impulse.
The next time you catch yourself touching your face, just stop for a moment, and think. How are you feeling: Anxious? Bored? Happy, Even? Or, was it in response to something that just happened? The more you think about the act and the feelings surrounding it, the more you can be mindful the next time.
4. Make your commute as safe as possible.
Are you driving to work? Keep disinfectant wipes in your car, so you can frequently rub down your steering wheel, radio dials, seat belt buckle, dashboard, anything!
If you’re using public transportation, you’ve got to be extra mindful—use the back of your lower arm or your elbow for opening doors, going through turnstiles, or riding the train. Carry a rag or a handkerchief for any moments when you can’t avoid grabbing handles or doorknobs.
5. Post visual reminders in your house and any house you’re going into regularly.
 At home, you’re more likely to let your guard down, wash your hands less, and touch your face more. Tape reminders to your fridge, walls, and doors about good hygiene practices. Above your sink, suggest a song to hum for the (at least) 20 seconds you need to spend washing your hands.
At home, you’re more likely to let your guard down, wash your hands less, and touch your face more. Tape reminders to your fridge, walls, and doors about good hygiene practices. Above your sink, suggest a song to hum for the (at least) 20 seconds you need to spend washing your hands.
Posting reminders around the home can be especially helpful if you’re in home care. It’s easier to control what happens in your own house, but if you’re going into a client’s, take the opportunity to do some education. After all, you’re a clinician and understand infection prevention protocols and how they can help both you and your client stay safe. Printing out tips and hanging them around their house is a great way to make them an ever-present reminder.
6. Manage visitor access (and suggest it to your home care clients).
While most people are social distancing and some states are enforcing shelter-in-place, the guidelines can be loose, and not everyone is taking it as seriously as they should. Think about that when you invite someone into your home. And encourage your clients think about it, too.
You may want to ask whether your guest has been out of the country or to an area of the US that is particularly dense with COVID-19 cases. Ask that your guests don’t come by if they’re feeling sick, especially if they have any symptoms that align with COVID-19.
7. Keep your work life and home life separate.
Leave a change of clothes near your door in the morning, so that you can take off your scrubs as soon as you get in and throw them in the laundry. Be smart when you’re cleaning your bag and supplies—as in, don’t do it while you’re preparing dinner and there are others in the kitchen.
8. Sanitize everything.
That includes your hands! Disinfect counters, remote controls, your keyboard and mouse, doorknobs, light switches, your phone—especially, your phone. Try and be mindful about the things you touch and how often.
9. Ask someone else to do the errands for you.
Sure, if the rest of your family is sheltering in place, it may seem more logical for you to stop at the grocery store on your way home. But don’t if you can avoid it. Ask if a family member or friend can help out or take advantage of delivery services. Your job is to care for other people and to keep them safe, and the more you’re out in public, the bigger your risk of infection.
10. Don’t come to work sick!
Now isn’t the time to ignore your health, grit your teeth, and endure. That’s dangerous for both you and those you are near. Stay home if you feel any of the symptoms of the Coronavirus and contact your doctor.
Those are our 10 tips for caregivers who are out there working from work during this health crisis. Thank you again—honestly, we can’t thank you enough. So, be mindful, stay safe, and take care of yourself.


Let Us Know What You Thought about this Post.
Put your Comment Below.